Osteoarthritis Treatment NYC by Marc Bystock L.Ac.
"Acupuncture is an effective treatment for Osteoarthritis. In my experience, I usually prescribed one to two visits weekly until the condition has improved and the pain has subsided. Then, a regular maintenance schedule may be customized for the patient to prevent flare ups."
-Marc Bystock L.Ac.
Contact Marc Bystock, Leading Holistic Acupuncturist in NYC for a Free Consultation.
CONTACT MARC
VERIFY YOUR HEALTH INSURANCE
Treatments for Osteoarthritis by NYC Acupuncturist in Midtown Manhattan NY 10016
What is Osteoarthritis?
Osteoarthritis is termed the common form of arthritis or the wear and tear type. It mostly affects adults, both middle aged and seniors. Over 54 million U.S. citizens have some form of osteoarthritis. Osteoarthritis means inflammation in the joint articulation, joint lining, cartilage and/or bone. The most common joints that become effected are the joints of the knees, hips, spine, hands and the big toe of the feet.
Approximately 50% of the general population will have knee osteoarthritis in their lifetime, and 25% will have hip osteoarthritis.
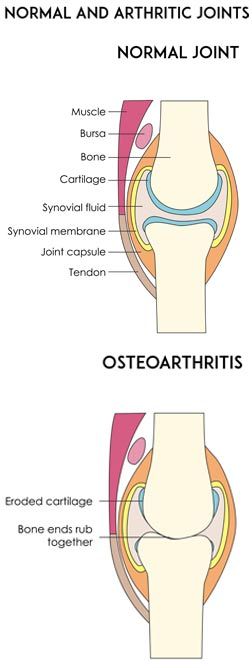
In a healthy state, a thin layer of firm and slippery cartilage cushions the space between bones. As the cartilage wears, bone rubs against bone causing friction and inflammation and pain. This is a condition of osteoarthritis. As more tissue becomes damaged, the immune system creates more inflammation to clean up the dead tissue. This process, unfortunately, causes more inflammatory damage which could spread around the body. If the joint tissue breaks down faster than the body can repair it, this may lead to permanent joint damage.
What Causes Osteoarthritis?
Not so long ago, Osteoarthritis was thought to be caused mainly by excessive wear and tear of the body at the affected areas. While it is still still true, excessive wear and tear can cause Osteoarthritis, science has expanded the common causes to include:
- Your genetics may have an influence
- Anyone obese or overweight may be at risk, excess weight causes too much physical stress bearing down on the joints
- Any persons who repetitively use the same joints over and over such as golfers, tennis players, or painters History of joint trauma, even if you had a joint injury years ago, it could result in osteoarthritis
- Multiple steroid injections
- The senior population is at higher risk because they have used their joints longer
- Birth defects, some people are born with malformed bone and cartilage that may lead to osteoarthritis later in life
- Hemochromatosis is a genetic metabolic disorder leading to the uptake and deposit of too much iron into the cartilage and joints resulting in arthritic condition
- Nutritional deficiencies such as calcium, magnesium, phosphorus, zinc, protein, iron, silicon, vitamins A, B, D, C, K, fatty acids, potassium, fluoride, boron
Common Symptoms of Osteoarthritis
Most people first notice an onset of Osteoarthritis because of pain, stiffness, or discomfort. All too often, it is when managing the pain and the related symptoms become too much to live with initiates a call to a doctor or health practitioner. Chances are, you will be experiencing one or many of these symptoms:
- Stiffness may occur
- Pain may happen with or without joint movement
- Tenderness and swelling may of the joint may occur
- Flexibility may diminish over time
- Crepitus may set in causing a crackling sound with movement
- Bone spur formation may occur
- Joint full range of motion loss may occur over time
A complete diagnosis can be made by palpation of the swollen joints, X-ray, Magnetic Resonance Imaging (MRI) and blood tests.
How Conventional Medicine Treats Osteoarthritis
The regular course of medical treatment for osteoarthritis include NSAIDS or non-steroidal anti-inflammatory over the counter medications. This classification of drugs provides anti-inflammatory and pain relief. These include aspirin, ibuprofen, and naproxen.
Treatment is palliative. Conventional medicine offers no cures for osteoarthritis. Over time the condition will only worsen. Therefore, case management is the only reasonable strategy.
It is necessary to keep the affected joint moving. Regular exercises like walking, biking, weight lifting, and swimming are all excellent to strengthen the surrounding joint supportive tissue and keep the joint lubricated.
Physical therapy may be prescribed to teach specific exercises and stretches to rebuild the surrounding areas and keep the joint active. With the condition worsening over time, the need for crutches, canes, and walkers may be needed as an external support mechanism.
The final stage may be surgery. Joint replacement has become a common practice in hospitals today. It is estimated that by the year 2029, 3.5 million knee replacement surgeries will be performed yearly in the United States alone. Today, there are approximately 500,000 total hip replacement surgeries performed annually. These joint replacement surgeries are being performed on a younger population over time. These patients have all come to end-stage arthritis.
A recent study indicates that people in their 50’s and 60’s with expectations to keep up and continue exercise activity may be one of the reasons that joint disease and joint replacement are on the rise.
Another possible factor is one less investigated, the rise in Lyme disease. Lyme disease is characterized by the Borrelia bacteria and other coinfections that parasitize joint cartilage for the continuance of their life cycle.
How Can Acupuncture Can Treat Osteoarthritis
Acupuncture is a powerful benefit in the treatment for osteoarthritis and must be considered. Acupuncture has been used for arthritis for thousands of years. It is part of Traditional Chinese Medicine that has evolved in ancient China. Traditional Chinese Medicine (TCM) consists of acupuncture, Pharmacopeia (Herbology), Tui Na (Massage) and Chinese dietetics (Nutrition). Acupuncture itself remains one of the most popular “alternative” medical modalities used throughout the world.
In Chinese medical terminology, acupuncture moves qi (energy) and blood. Both of which may become stagnated or blocked in cases of osteoarthritis resulting in a bi-syndrome or inflammation and pain.
There is an overwhelming amount of medical research that shows that when an acupuncture needle is correctly placed, it sets off a cascade of events. A signal runs from the pain site ascending the spinal column to the brain. This triggers a series of neurotransmitters, endorphins, enkephalins, and endocannabinoids to be released. These naturally produced opioid-like chemicals reduce and block pain inside of the body. In addition, acupuncture provides a boost in cortisol production, which is the body’s own anti-inflammatory.
Acupuncture also provides blood perfusion, which increases oxygen and nutrients to the affected tissue, lowering inflammation, and providing healing support. Acupuncture is an effective therapy and is usually prescribed as one to two visits weekly until the condition has improved. Then a maintenance schedule may be customized for the patient.
In my practice, the typical osteoarthritic patient would take pain relieving and anti-inflammatory herbs and supplements in addition to acupuncture treatments. A special non-inflammatory food program would be implemented as well as stretching and specific exercises to increase the patient’s joint mobility.
Primarily because osteoarthritis has become so prevalent, I have had a lot of experience treating this type of patient. Each case is unique, and patient outcomes may vary. In most cases, patients find pain relief with anti-inflammatory benefits. Best results occur when patients are treated for early-stage symptoms. Later stage cases can also be helped as the strategy is usually set to slow down the progression of the disease and break the pain cycle without any side effects.
Anyone who has had to go through the extensive process of joint replacement surgery also needs acupuncture treatments post-surgery. This helps to lower the pain brought on by surgery. Acupuncture also promotes the healing of scar tissue produced by the surgery. If left untreated scarring will block energy (qi) and blood flow to both local and distal areas.
Understand that just because the arthritic joint tissue has been removed doesn’t mitigate the fact that the underlying reasons for inflammation and the tissue destruction may continue systemically attacking other joints. It is still necessary to lower the painful inflammation process, and acupuncture is excellent at doing just that.
Contact NYC Acupuncturist Marc Bystock L.Ac. for a Free Consultation Regard Osteoarthritis Treatment
I am sometime surprised by long a person will simply live with the pain and discomfort of Osteoarthritis, instead of going to an experienced and qualified health practitioner as the first symptoms appear.
Luckily, the human body has amazing powers of restoring itself back to a healthy state, and I sincerely believe I can help you accomplish just that. My holistic treatments are custom-designed to address the exact needs of your body, and implement a healing protocol that is as fast as it is effective.
I hope you contact me for a free consultation, so I may review your condition more carefully and advise you as to what I believe is the best process for restoring your body to an arthritis-free life.
Please contact me
today!