Rheumatoid Arthritis Treatment NYC by Marc Bystock L.Ac.
"I understand the harmful effects of arthritis all too well. A few years ago, I went through the personal struggles of having arthritic symptoms, and made a complete recovery. I can help you too!."
-Marc Bystock L.Ac.
Contact Marc Bystock, Leading Holistic Acupuncturist in NYC for a Free Consultation.
CONTACT MARC
VERIFY YOUR HEALTH INSURANCE
Treatments for Rheumatoid Arthritis Pain Relief by NYC Acupuncturist in Midtown Manhattan NY 10016
What is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is a chronic inflammatory disease that affects the joints of the body, causing joint pain, redness, stiffness, swelling, and lack of joint mobility. Rheumatoid is classified as an autoimmune disorder having the immune system attack its own self tissue. It affects over 1.5 million people living in the United States, and over three-quarters of those people are women. RA most often begins between the ages of 30 and 60, years old, although it’s possible to start at any time.
Rheumatoid arthritis typically attacks the joints and joint lining of the hands, knees, and feet. It is often worse in the morning hours, with the condition improving as movement increases throughout the day. Most often, RA affects the same joints bilaterally.
Rheumatoid Arthritis can become systemic, spreading around the body like a wildfire, even attacking bodily organs like the lungs, skin, eyes, heart, blood, nerves, or kidneys. In addition, those affected may feel fatigued throughout the day and an understanding that they generally do not feel well.
Causes of Rheumatoid Arthritis
A predisposition to your family genetics could increase one’s risk of getting Rheumatoid Arthritis. Other factors leading towards RA include being obese, smoking cigarettes, being a female, and living past 60 years of age.
Once you have Rheumatoid Arthritis, you will have it for life. The severity of the symptoms of RA may vary depending on the multiple lifestyle factors, especially one’s overall health.
The causes of Rheumatoid Arthritis and the autoimmune disease itself are not well understood by conventional medicine. Genetics are often involved, as well as:
- An inefficient working immune system may be at fault.
- Environmental factors causing toxicity to build up in the body
- Hormonal dysregulation
- Chronic high-stress levels
- An inflamed digestive tract (dysbiosis)
- Dysglycemia (poor blood sugar regulation)
- Cardiovascular disease
Any of these factors can move the immune system from a Th1 state to a Th2 dominant state boosting Th17 status and the progression towards an autoimmune condition.
Symptoms of Rheumatoid Arthritis
RA symptoms typically come and go from total remission to a massive flare-up signaling pain and inflammation.
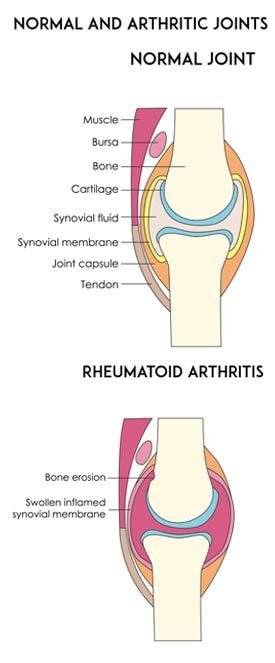
Joint cartilage serves to prevent friction between bones. It acts as a shock absorber allowing joint movement to occur more smoothly and without pain. With Rheumatoid Arthritis comes a great deal of inflammation, causing the cartilage to break down and wear away. Eventually, joints may fuse to protect against further erosion. Other common symptoms include:
- Joint inflammation, swelling, redness, stiffness
- Pain may be worse in the morning
- Fatigue (sleeping a lot)
- Not feeling well
- Poor appetite
- Fever
Rheumatoid arthritis increases the risk of having other disorders:
- Osteoporosis-a condition of brittle bones that may become weak and fracture
- Sjogren’s syndrome-an autoimmune disorder causing dry mouth and dry eyes
- An overall increase in infections
- An increase in measured body fat percentage
- Carpal tunnel syndrome-an increase in pressure on the nerve that serves the wrist causing pain and lack of movement in the wrist joint
- Cardiovascular disorders-RA can increase the inflammation surrounding the heart
- Lung disease-RA can lead to an increase in inflammation of the lung tissue causing shortness of breath
How is Rheumatoid Arthritis Diagnosed?
Rheumatoid Arthritis can be challenging to diagnose in the early stages because it can mimic other diseases. Your healthcare provider should examine your joints for range of movement and flexibility, redness, swelling, and muscle strength. Blood and imaging tests should be ordered from a medical laboratory, including:
- An Erythrocyte sedimentation rate (ESR)-may indicate inflammation
- C-reactive Protein (CRP)-may indicate systemic inflammation
- Rheumatoid Factor-measures rheumatoid proteins in your blood
- Anti-cyclic citrullinated peptide (anti-CCP) an antibody in most rheumatoid arthritis patients
- Magnetic Resonance Imaging (MRI) may look for the severity of systemic tissue damage
- X-Ray-can look and track the progression of arthritis in the joints and surrounding structures
What is the Conventional Treatment for Rheumatoid Arthritis?
Both researchers and clinicians agree that there is no cure for Rheumatoid Arthritis. However, remission is a real goal which will keep symptoms low and the patient comfortable without pain or flare-ups.Nonsteroidal anti-inflammatory drugs (NSAIDS) can be used to dampen inflammation and pain. NSAIDS are over the counter medications. Their side effects include gut inflammation and kidney disease.
Corticosteroids like prednisone are prescribed to lower inflammation, pain, and slow down joint damage. Their side effects include thinning of bones, gaining excess weight, and diabetes type 2 disorder.Disease-modifying anti-rheumatic drugs (DMARDs) include methotrexate, which is used to slow down the inflammatory and joint destructive processes.
Biological Medications are also known as biological response modifiers include Humira and Embrel. These drugs are selective at making specific changes in the pathways of the immune system. The intended outcome is to lower inflammation and joint damage. Side effects include an increase in infections and the possibility of blood clots in the lungs.
Physical therapy may be prescribed to learn new exercises that may strengthen the affected area and benefit the surrounding tissue. Surgery is the last step if all of the above measures fail. The surgical removal of inflamed synovial tissue that surrounds the joint is termed a splenectomy.
If a tendon becomes weakened or tears, then tendon surgery may be required. Surgery may be required to fuse joints whenever a joint replacement is not appropriate.
A joint replacement is the last measure to repair the inflammatory damage of Rheumatoid Arthritis. The necrotic or damaged joint is surgically removed and replaced with a prosthesis which may be made from metal and plastic. The number of total hip and knee replacement surgeries are on the increase as the number of RA and osteoarthritis patients is increasingly multiplying.
How I Use Holistic Acupuncture to Treat Rheumatoid Arthritis
Acupuncture is part of the Traditional Chinese Medicine system (TCM). These natural medical modalities date back several thousand years. Acupuncture uses very thin needles inserted into specific acupoint locations in the body resulting in an anti-inflammatory response that lowers pain.
Acupuncture effectively triggers several neurotransmitters, enkephalins, endorphins, and endocannabinoids that naturally block and lower both pain and inflammation. In addition, acupuncture treatments can lower body stress and support blood perfusion. Moving more blood brings additional nutrients and oxygen to the affected tissue.
One published study of 54 Rheumatoid Arthritis participants showed that 100% of the individuals improved their condition. Other research coming out of Russia using electro-acupuncture on Rheumatoid Arthritis showed improvement across the board as was documented by blood tests taken before and after the study.
I understand the harmful effects of arthritis all too well. A few years ago, I went through the personal struggles of having arthritic symptoms. Today, through trial and error, I’ve learned how to manage my arthritic conditions, keep the inflammation low. I have applied those same lessons to the many arthritic patients that I treat weekly in my office. I want to give my patients every opportunity possible to lower their inflammation and pain, decrease stress, and promote healing.
- Acupuncture-lowers pain and inflammation promotes relaxation, regulates hormones and perfuses blood
- Herbology, the use of herbs to block and lower inflammation and pain pathways
- Vitamin and mineral supplements to fill in nutritional deficiencies, to promote tissue healing and support the resolution of inflammation.
- Cold laser therapy-to lower inflammation and decrease pain
- Topical herbal medications to lower inflammation, pain, and increase blood flow to the affected area.
- Bioenergetics to increase blood flow systemically includes PEMF
- Specific food plans to lower inflammation and optimize health
Contact NYC Acupuncturist Marc Bystock L.Ac. for a Free Consultation Regarding Rheumatoid Arthritis Treatments
If you or anyone you know may suffer from the negative effects of Rheumatoid Arthritis, I can help! Don’t wait, time is of the essence as joint damage continues.
Contact me as soon as possible for a free consultation to see how acupuncture and my natural therapies can help lower your pain and inflammation and manage your Rheumatoid Arthritis!
Please contact me
today!